Since its inception, the Affordable Care Act (ACA) has provided millions of men, women and children with direct, convenient access to essential health coverage and prescription medications. But this law has also benefited the American workforce. Perhaps more than any other field, the ACA has jumpstarted healthcare employment.
But with so many new and existing beneficiaries, is the healthcare industry prepared? Actually, the ACA has taken great pains to ensure the healthcare workforce can handle this wave of patients. The law’s Title V section includes more than 40 provisions to support, increase and encourage innovation. These will enable healthcare workers to provide care for more patients in more proactive ways, such as student loans, training grants and programs for care delivery and employee retention.
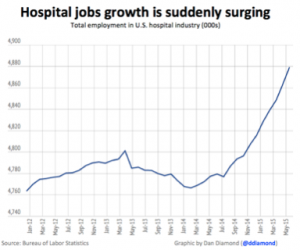
From 2012 to 2014, hospital hiring was flat. But with the ACA’s passing, healthcare jobs have become an engine of opportunities. The most recent jobs report released (June 5th) was the 10th straight month of jobs growth for hospitals AND the 14th month of jobs gains in the past 15. Typically, hospitals are major employers, providing the surrounding area with jobs. According to the Bureau of Labor Statistics, the last year has seen an increase of more than 100,000 hospital-related jobs, the biggest since 2008. The chart below spotlights this hospital employment increase.
The role of the Affordable Care Act
Studies show that the U.S. economy has been improving since March 2010. Since the recession, the entire private sector gained 12.3 million jobs, including many for healthcare. But the ACA has played a very important role, especially over the past year. This is due to the law’s two-pronged strategy for expanding coverage: 1.) the launch of the insurance exchanges; and 2.) the growth of the Medicaid program. The number of uninsured Americans decreased to about 11 percent, a record low. Hospitals now have less bad debt and more revenue, with many experiencing their best financial performance in years.
Still, the ACA’s impact can’t be ignored, as taxes collected fund the creation of millions of new healthcare jobs.
Aside from improving healthcare job training, this helps to create new jobs in the health insurance marketplace and health education. The ACA also fuels employment by enabling small businesses to provide better health benefits, thereby making the available jobs more desirable.
Funding programs for healthcare providers
The ACA’s been a staunch supporter of America’s health care workforce, as doctors, nurses, and other health care providers are its backbone. The ACA increased funding to the National Health Service Corps (NHSC), which offers healthcare providers financial, professional and educational resources, in exchange for working in traditionally underserved areas of the country. The ACA also created Health Professions Opportunities Grants, providing tuition and supportive services for those seeking training in health professions. To date, more than $67 million has been awarded to low-income individuals to attend training programs to enter the healthcare workforce.
The recession affected the public health workforce, but the ACA has been able to increase budgets and hiring. The ACA established the Prevention and Public Health Fund, which targets health promotion, disease prevention, early screening and management of chronic conditions. Between 2010 and 2012, more than $2 billion was allocated, including funding for programs aimed at expanding and developing the healthcare workforce, such as:
- 500 additional primary care residency slots
- Training for more than 600 new physician assistants
- 10 new clinics run by nurse practitioners (NPs) and to assist in new NPs’ clinical training
- Funds for states to develop their own strategies to expand their primary care workforces
- More than $40 million to support 37 nationwide Public Health Training Centers (university-based facilities
- providing education and training for public health practitioners)
- Funding to nursing schools for stipends to increase full-time enrollment
- $45 million in funding to bolster state health departments’ epidemiology, laboratory, and health
- information systems, including hiring and staff training
The ACA has made major efforts in establishing federally qualified health centers, also called community health centers (CHCs). These are essential in achieving the law’s goal of moving toward a wellness model of service provision. CHCs are the nation’s largest primary care provider network, serving low-income Americans with no or public insurance. The ACA allocated $11 billion through 2015, with the goal of doubling the number of patients these facilities are able to serve to 40 million. To date, CHCs have increased employment by 15 percent, including more than 25,000 new full-time positions.
This healthcare law has allocated $200 million over four years to improve and expand school-based health centers, which link schools and community health organizations. These facilities enable children with acute or chronic illnesses to attend school , while also providing health promotion and screening and prevention services. The ACA seeks to help these centers nearly double the number of children they serve, while also creating new jobs for healthcare providers.
Another ACA-driven initiative is using less-expensive providers in more effective ways. For example, the ACA recommends receiving primary care from nurse practitioners, physician’s assistants and registered nurses. The improvement of the management of chronic conditions (cancer, diabetes, etc.) is also a major goal, as these diseases account for 75 percent of U.S. healthcare dollars.
It is the ACA’s overlying goal to make and keep people healthier by providing high quality, cost-effective services that everyone can access. And in the event the law is repealed or changed, these various new care delivery programs care are expected to continue.
Sources:
http://www.forbes.com/sites/dandiamond/2015/06/05/hospitals-jobs-growth-is-suddenly-booming/
http://obamacarefacts.com/impact-of-obamacare-on-jobs/